The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) gathered the Drug-related infectious diseases (DRID) expert network to share the latest developments on drug-related infectious diseases in Europe and to identify steps needed to improve the production, availability and use of public health-oriented information at the European level.
The DRID network brings together national experts nominated by national focal points of the EU Member States, Norway and Turkey, as well as institutional partners (ECDC, WHO, Correlation). The meeting also welcomed experts from the Western Balkans (IPA7 project), the European Neighbourhood Policy countries (EU4MD project), Georgia, the United Kingdom, Australia and the United States. Participating experts come from ministries of health, public health institutes, drugs agencies, health services, universities, research institutes and civil society.
The group held an online meeting on 26-27 October 2021, focusing on:
- The direct impact of COVID-19 on people who use drugs and the COVID‑19 vaccination campaign among this group;
- A review of recent HIV trends and outbreaks, as well as infectious endocarditis linked to injecting drug use with a focus on risk factors and control measures in place;
- Country experiences in the elimination of viral hepatitis as a public health threat among people who inject drugs (PWID) and related EMCDDA projects, with a focus on harm reduction and the continuum of care.
The report section on Outbreaks includes some interesting information from South East Europe.
In 2011, an HIV outbreak among PWID was detected in Athens, Greece (Paraskevis et al., 2011). After a combination of prevention and ‘seek-test-treat’ interventions were implemented (including scaled-up NSP, testing, linkage to AOT and antiretroviral treatment (ART), HIV incidence declined (Sypsa et al., 2017) from 7.8/100 person-years in 2012 to 1.7/100 person-years in 2013. However, preliminary data from the latest round of the ARISTOTLE study, conducted in 2018-20 (Roussos et al., 2021) among 681 PWID who were included in previous rounds, suggest that HIV prevalence increased from 14.2 % (2012-13) to 22 % (2018-20). While incidence estimates never returned to their 2011-12 levels, they ranged from 1.52 to 2.04/100 person-years, indicating ongoing transmission. The prevalence of homelessness (25.6 %) and cocaine injecting (28.1 %) had increased over the period. Predictors of seroconversion included lower education, larger network size and daily drug use. The authors concluded that the current level of prevention and treatment services was below levels that would be required to bring transmission down to pre-outbreak levels. They also noted that the COVID‑19 pandemic has severely impacted HIV prevention services for PWID, which could increase the risk of HIV transmission in this population. The study team conducted a similar study in Thessaloniki, the second-largest city in the country, where 1 101 PWID were recruited during 2019-20. They found high HIV incidence among the study population, suggesting that an outbreak was occurring at a time when COVID‑19 controls measures were in place. The authors highlighted that immediate interventions were required to control transmission.
Following the DRID meeting, national experts from three additional EU countries have reported signals of increased HIV transmission among people who use drugs. In Sofia, Bulgaria, reports indicate that the pandemic seems to have worsened a situation that was already deteriorating with respect to harm reduction funding. According to data from the laboratory at the State Psychiatric Hospital for Treatment of Drug Addiction and Alcoholism in Sofia, reported by the national expert, the positivity rate for HIV infection among PWID in the capital of Bulgaria was significantly higher in 2019-20 (12.8-14.5 %) than in the previous years (when positivity rates were between 3-6 %). A parallel increase in HBV positivity (HBsAg) was also noted from 2019 (5.9 %) to 2020 (7.6 %). This comes after the Global Fund ended its financial support to harm reduction services in 2017. It consequently led to a disruption in needle and syringe programmes, and a reduction by more than half in the number of PWID being tested annually. The National Centre of Public Health and Analysis is organising a meeting with stakeholders and decision-makers to initiate legal changes in order to ensure sustainable financial support for harm reduction services.
The national expert from Slovenia reported that, by November 2021, four new HIV diagnoses among PWID were reported to the National Institute of Public Health among a total number of 28 reported new HIV diagnoses during 2021. This raised concerns that HIV infections might have started to spread more during the COVID‑19 pandemic among PWID in the country. Since 1986, when HIV reporting became mandatory in Slovenia, a total of 29 HIV infections among PWID have been reported, and such a high number of cases (four) were reported only once before, in 1996. The importance of reaching a good coverage of harm reduction services for PWID was re-emphasised.
To read full report from this meeting and get the information from expert update, follow this link>>>.






 Over 11 million people are imprisoned worldwide today, the highest number ever recorded. One in five people in prison worldwide is held for drug offences, and 90% of people who inject drugs will be incarcerated at some point in their life. People in prison are at greater risk of HIV, hepatitis C, tuberculosis and COVID-19. When they are released from prison, their risk of overdose increases by up to 69-times.
Over 11 million people are imprisoned worldwide today, the highest number ever recorded. One in five people in prison worldwide is held for drug offences, and 90% of people who inject drugs will be incarcerated at some point in their life. People in prison are at greater risk of HIV, hepatitis C, tuberculosis and COVID-19. When they are released from prison, their risk of overdose increases by up to 69-times.

 As a criminalised population, sex workers have been disproportionately impacted by the COVID-19 pandemic, often living in precarious economic situations and excluded from social protection systems. The policy brief COVID-19 and Sex Workers/Sex Worker-led Organisations, produced by the Global Network of Sex Work Projects (
As a criminalised population, sex workers have been disproportionately impacted by the COVID-19 pandemic, often living in precarious economic situations and excluded from social protection systems. The policy brief COVID-19 and Sex Workers/Sex Worker-led Organisations, produced by the Global Network of Sex Work Projects (
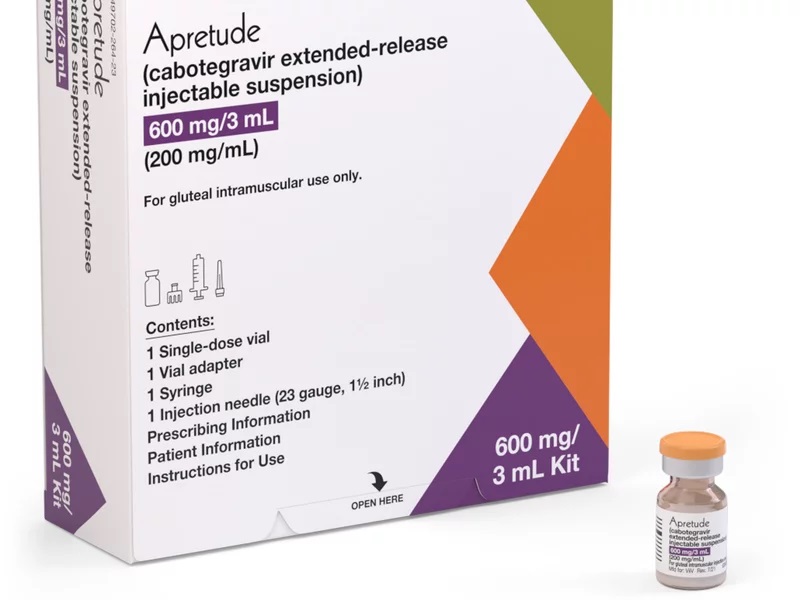
 The United States Food and Drug Administration announced its first approval of a long-acting HIV prevention medication on 20 December 2021. The long-acting injectable cabotegravir (CAB – LA) is approved as a pre-exposure prophylaxis (PrEP) for adults and adolescents who are at risk of acquiring HIV sexually in the United States of America. Apretude is given first as two initiation injections administered one month apart, and then every two months thereafter. Patients can either start their treatment with Apretude or take oral cabotegravir (Vocabria) for four weeks to assess how well they tolerate the drug.
The United States Food and Drug Administration announced its first approval of a long-acting HIV prevention medication on 20 December 2021. The long-acting injectable cabotegravir (CAB – LA) is approved as a pre-exposure prophylaxis (PrEP) for adults and adolescents who are at risk of acquiring HIV sexually in the United States of America. Apretude is given first as two initiation injections administered one month apart, and then every two months thereafter. Patients can either start their treatment with Apretude or take oral cabotegravir (Vocabria) for four weeks to assess how well they tolerate the drug.![Drug Decriminalisation [e]Course](http://dpnsee.org/wp-content/uploads/2021/12/eCourse.jpg)