Injecting drug use remains a crucial risk factor for acquiring blood-borne viruses such as hepatitis B and C, and HIV, but also other infectious diseases, such as sexually transmitted infections (STIs) and tuberculosis (TB). While for STIs and TB, injecting drugs does not directly cause infection, factors such as living conditions or higher-risk sexual practices place some people who inject drugs at a greater risk.
In new public health guidance released today, the European Centre for Disease Prevention and Control (ECDC) and the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) have joined forces to identify key interventions to address infectious diseases in this population. Reflecting on new evidence, infectious disease treatments, and public health concepts, this guidance updates the 2011 edition.
This joint guidance reinforces the need for a comprehensive and coordinated approach to addressing the persistent public health challenge of drug-related infections in EU/EEA countries. Ultimately, it aims to improve the well-being and health outcomes of individuals affected by these issues.
The guidance aims to support policy-makers and public health/social programme planners by providing an evidence base for developing national strategies, policies, and programmes for preventing and controlling infections and infectious diseases among people who inject drugs. It also provides practice considerations and aims to inform the monitoring and evaluation of prevention and control strategies, policies, and programmes.
The six key intervention areas and recommendations proposed in the guidance range from the provision of sterile injection equipment, testing, and vaccination, to the treatment of infections and drug dependence. They are:
- Sterile injection equipment – provide sterile needles and syringes and other drug preparation equipment (cookers, filters and water for injection), including in prisons and through pharmacies.
- Drug dependence treatment – provide opioid agonist treatment (OAT), including in prisons, for people who are dependent on opioids. OAT should be offered in conjunction with sterile injecting equipment and information, education, and counselling.
- Vaccination – offer vaccinations against hepatitis A and B, respiratory infections and tetanus, as well as the pneumococcal and the human papillomavirus vaccines for people living with HIV who inject drugs.
- Testing – routinely offer voluntary and confidential infectious disease testing and link all people with a positive test result to care.
- Infectious disease treatment – offer infectious disease treatment according to national and international guidelines, ensure there is good cooperation and links between service providers dedicated to people who inject drugs and infectious disease care; involve peer mentors to strengthen adherence to treatment.
- Drug consumption rooms – provide supervised injecting facilities to reduce injecting risk behaviour among people who inject drugs, which could as a consequence contribute to the prevention of HCV and HIV transmission.
To access the Guidance follow this link>>>.


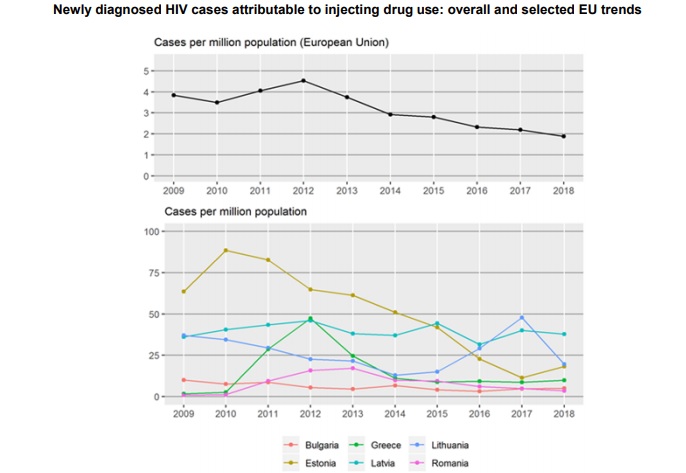
 Launched during European Testing Week (15–22 May), the report offers an overview of drug-related infectious diseases among PWID in Europe, including the prevalence and incidence of HIV and viral hepatitis. It also tracks progress on health targets and showcases successfully implemented evidence-based interventions. It underlines the need to ramp up prevention and testing and signals that European countries are lagging behind when it comes to treating hepatitis C virus (HCV) and HIV among PWID.
Launched during European Testing Week (15–22 May), the report offers an overview of drug-related infectious diseases among PWID in Europe, including the prevalence and incidence of HIV and viral hepatitis. It also tracks progress on health targets and showcases successfully implemented evidence-based interventions. It underlines the need to ramp up prevention and testing and signals that European countries are lagging behind when it comes to treating hepatitis C virus (HCV) and HIV among PWID. To read full report,
To read full report,